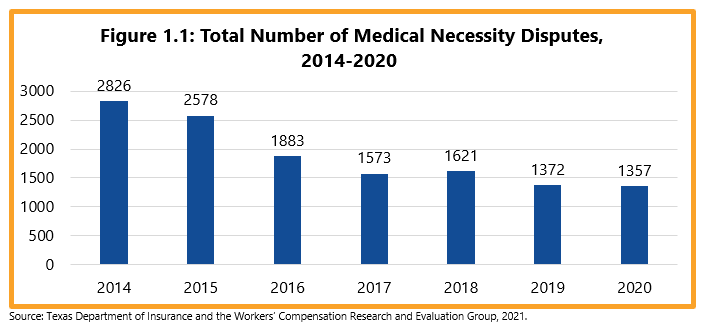
Key findings
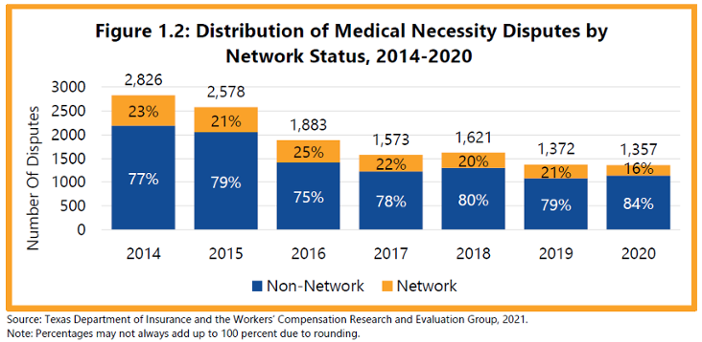
Non-network claims account for most medical necessity disputes (about 8 out of 10). The proportion of medical disputes for network claims was between 20 and 25 percent from 2014 to 2019, and then dropped to 16 percent in 2020. Although almost half of new workers’ compensation claims are treated in networks, network medical necessity disputes are less frequent since networks contract with health care providers and those contracts include requirements to follow the network’s treatment guidelines and preauthorization requirements.
Generally, there are three types of medical disputes in the workers’ compensation system:
- fee disputes - disputes over the amount of payment for an injured employee’s medical services;
- preauthorization disputes/concurrent review medical necessity disputes - disputes about the medical necessity of future or current medical treatments that the insurance carrier denied; and
- retrospective medical necessity disputes - disputes about the medical necessity of treatments already provided and billed.
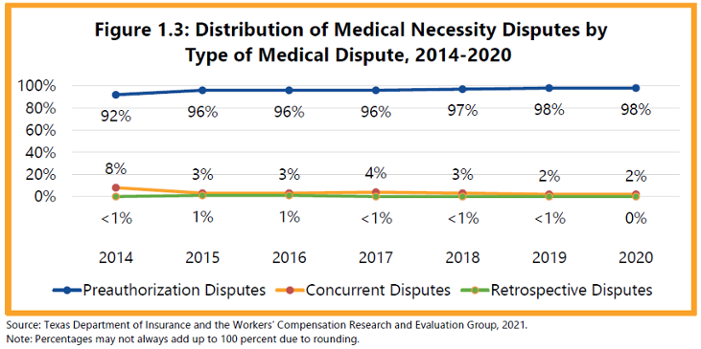
Most medical necessity disputes in recent years (more than 9 out of 10) were associated with preauthorization denials. Concurrent review disputes declined (from 8 percent in 2014 to 2 percent in 2020), and retrospective medical necessity disputes only represented about 1 percent of medical necessity disputes. In 2020, health care providers and injured employees did not request any retrospective medical necessity dispute.
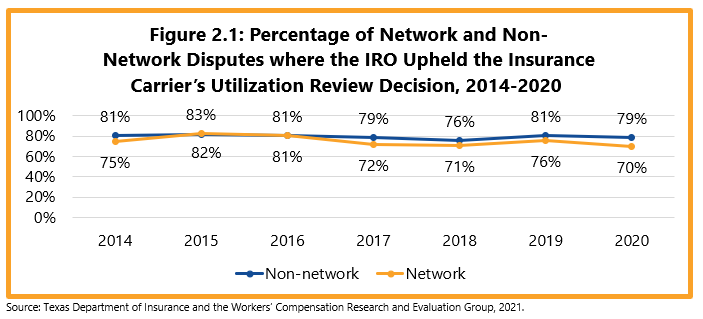
As part of the 2001 and 2005 legislative reforms, the Texas Legislature required the use of evidence-based treatment guidelines by health care providers and insurance carriers to provide guidance on what medical services were appropriate for specific work-related injuries. As a result, most medical necessity disputes resulted in decisions that upheld the insurance carrier’s utilization review denial. In 2020, about 70 percent of disputes involving network claims and 79 percent of disputes involving non-network claims upheld the insurance carrier’s utilization review decision.
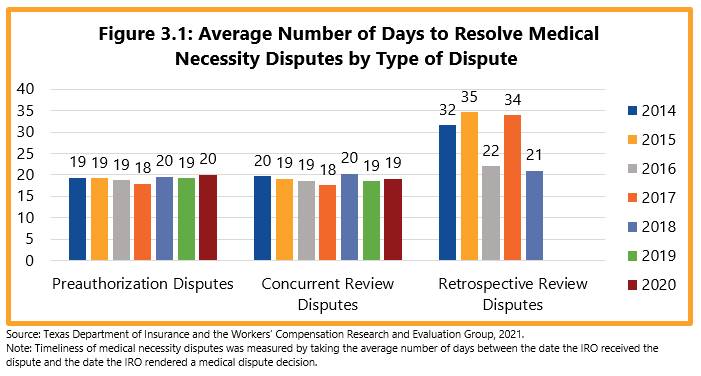
The mean time frame to resolve preauthorization and concurrent review medical necessity disputes was between 18 and 20 days. While the mean time frames to resolve retrospective medical necessity disputes varied over time, these disputes are infrequent. IROs received three retrospective review disputes in 2019 but did not render a decision on them. No retrospective review dispute was filed in 2020.